Machine learning meets medicine in the fight against superbugs
Modeling how MRSA bacteria spread on the body can enhance treatments.
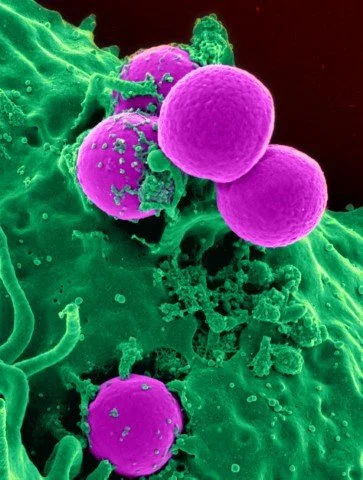
Scanning electron micrograph of a human neutrophil ingesting MRSA. Image: National Institute of Allergy and Infectious Diseases, National Institutes of Health on Flickr, CC BY-NC 2.0
MRSA is an antibiotic-resistant staph infection that can be deadly for those in hospital care or with weakened immune systems. Staphylococcus aureus bacteria live in the nose without necessarily producing any symptoms but can also spread to other parts of the body, leading to persistent infections. Management of MRSA is long-term and laborious, so any steps to optimize treatments and reduce re-infections will benefit patients. This new research can predict how effective different treatments will be by combining patient data with estimates of how MRSA moves between different parts of the body. The study was published in Journal of the Royal Society Interface in July 2022.
The researchers compared data from 2000 patients with MRSA after hospital visits. In one group, patients were given standard information about how to treat MRSA and prevent its spread. The second group followed a more intensive ‘decolonization’ protocol to eliminate MRSA through wound disinfection, cleaning the armpits and groin, and using nasal spray. Both groups were tested for MRSA on different body parts at various time points over nine months.
The current state-of-the-art in medical research often involves comparing two groups in this way, to see if an intervention or treatment could be effective. The new study added another element: a mathematical model that looked at the interactions between treatments and body parts. “The model shows how MRSA moves between body parts,” says senior author Pekka Marttinen, professor at Aalto University and the Finnish Center for Artificial Intelligence FCAI. “It can help us optimize the combination of treatments and even predict how new treatments would work before they have been tested on patients.”
Based on the patients’ MRSA tests—whether bacteria were present in the nose, skin, throat or wounds over time—the researchers could calculate the probability that an infection will move to another part of the body, depending on the patient’s treatment group. There was less internal transmission of MRSA around the body in the decolonization group, for example. “Decolonization itself works,” says Marttinen, “but out of all the treatment protocols we wanted to know, can we find the best or simplest way to get rid of MRSA?”
The model confirmed that MRSA spreads primarily from the nose. The nasal spray by itself was found to be very effective, but the model also showed that nasal spray plus disinfecting mouthwash was a more powerful combination against MRSA. “In fact,” comments first author Onur Poyraz, a doctoral researcher at Aalto, “each different treatment had a positive contribution to the clearance of MRSA, which is something we could only discover and quantify through this model.” The results also provide a pathway for drug development to improve the treatments and medicines used for MRSA decolonization; for example, enhanced skin disinfection with either nose spray or mouthwash could virtually eliminate MRSA in a hypothetical scenario. “Using a mathematical model allows to investigate all the different parts of a clinical protocol, hopefully contributing to the design of more efficient treatments and giving better guidance for doctors,” says Poyraz.
A follow-up to this research, from the same research group, will examine the genomes of MRSA and how they contribute to the efficiency of the treatments.
Reference: Poyraz O, Sater MR, Miller LG, McKinnell JA, Huang SS, Grad YH, Marttinen P. Modelling methicillin-resistant Staphylococcus aureus decolonization: interactions between body sites and the impact of site-specific clearance. Journal of the Royal Society Interface. doi: 10.1098/rsif.2021.0916